CKD Stages: Understanding the Stages of Chronic Kidney Disease
Chronic Kidney Disease (CKD) is a medical condition characterized by gradually losing kidney function over time.
The kidneys play a crucial role in filtering waste products and excess fluids from the blood, regulating blood pressure, and maintaining a balance of electrolytes in the body. CKD can develop slowly over an extended period, often without noticeable symptoms in its early stages.
CKD is typically categorized into different stages based on the estimated glomerular filtration rate (eGFR), which measures how well the kidneys filter waste and excess fluid from the blood.
Understanding the CKD stages and potential chronic kidney disease symptoms helps assess the severity of the disease and determine the most appropriate treatment options available.
If you or a loved one are living with chronic kidney disease, our team is here for you.


What Causes Kidney Failure?
Proper kidney function is vital for overall health.
The kidneys are essential organs that filter waste, help maintain fluid balance, regulate blood pressure, maintain electrolyte balance, control pH levels, and produce hormones that tell our body to make red blood cells. When they are injured or failing, it can affect various aspects of our total health and well-being.
Kidney failure, or renal failure, occurs when the kidneys lose their ability to effectively filter waste products and remove excess fluids.
Acute kidney failure is a rapid and often reversible loss of kidney function.
Common causes include:
- Dehydration
- Severe infections like sepsis
- Blockages in the urinary tract, such as kidney stones or an enlarged prostate
- Exposure to certain medications, heavy metals, or toxins
- Physical injuries to the kidneys
- Severe bleeding
Chronic kidney disease is characterized by a gradual loss of kidney function over time and can result from various underlying conditions, including:
- Diabetes
- High blood pressure
- Glomerulonephritis – inflammation of the glomeruli (the kidney’s filtering units)
- Polycystic kidney disease (PKD) is a genetic condition where fluid-filled cysts develop in the kidneys.
- Autoimmune diseases like lupus and specific vasculitis disorder
- Chronic kidney infections

Symptoms of Kidney Failure
In the initial stages of kidney disease, many individuals may not experience noticeable symptoms. However, it’s essential to recognize that chronic kidney disease can silently progress and cause harm even when you feel well.
Symptoms of CKD and kidney failure can vary from person to person, but may include:
- Overwhelming fatigue
- Nausea and episodes of vomiting
- Difficulty with concentration or experiencing confusion
- Swelling (edema), particularly noticeable in the hands, ankles, or face
- Increased frequency of urination
- Muscle cramps or spasms
- Dry or itchy skin
- Reduced appetite or a metallic taste in your mouth

The Role of GFR
The glomerular filtration rate (GFR) is a critical diagnostic marker and measurement used to assess kidney function and determine the stages of CKD.
GFR provides valuable insights into how effectively the kidneys filter waste products and excess fluids from the bloodstream.
The GFR is typically expressed in milliliters per minute per 1.73 square meters (mL/min/1.73m²) of body surface area. This specific unit of measurement is used to standardize GFR values across individuals of different body sizes.
To understand the role of GFR in CKD diagnosis and staging, it’s important to note that as kidney function declines, the GFR decreases. The severity of CKD is categorized into stages based on the GFR value.

Stages of CKD and Progression
There are five stages of kidney failure primarily categorized by the GFR. Each stage reflects the severity of kidney damage and is associated with specific symptoms, causes, and risk factors.
CKD stages are as follows:

Chronic Kidney Disease Treatment Options
CKD treatment and management vary depending on the stage and severity of the condition.
For advanced CKD stages, two primary treatment options are dialysis and kidney transplant.
Dialysis
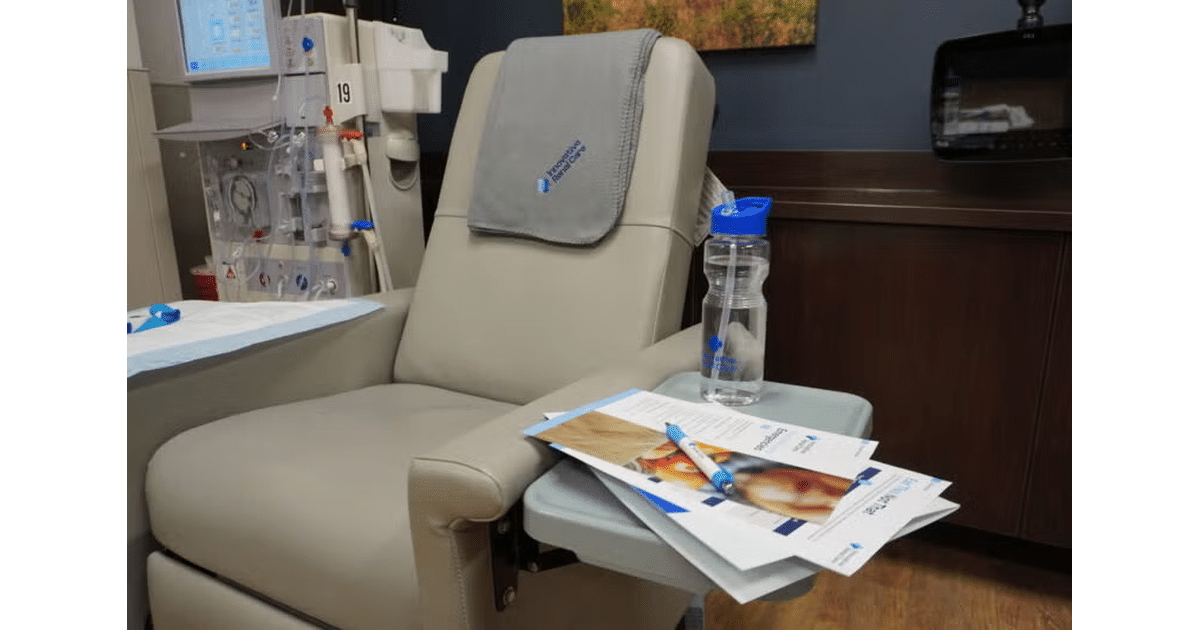
Dialysis is a life-sustaining treatment for individuals with end-stage kidney failure.
There are two main types of dialysis:
- Hemodialysis: In hemodialysis, the patient’s blood is filtered outside the body through a machine that removes waste and excess fluids and returns the filtered blood to the body. This process typically takes place at a dialysis center several times a week.
- Peritoneal Dialysis: Peritoneal dialysis (PD) uses the patient’s abdominal lining (peritoneum) as a natural filter. A sterile solution is introduced into the abdomen through a catheter, and waste products are drawn out through this solution, a process known as an exchange.
Both types of dialysis:
- Provide life-sustaining treatment when kidney function is severely impaired.
- Are accessible in many regions, offering regular treatment sessions without waiting on a suitable donor.
Kidney Transplant
A kidney transplant involves the surgical implantation of a healthy kidney from a living or deceased donor.
This is considered the best treatment option for individuals with end-stage kidney disease because it can restore normal kidney function, eliminating the need for dialysis. However, finding a suitable donor and undergoing the transplant surgery are complex processes.
The choice between dialysis and kidney transplant depends on individual circumstances, including the patient’s health, lifestyle, and the availability of a suitable donor.

Effective Care for All Stages of Chronic Kidney Disease
Early detection, management, and treatment are essential in all stages of chronic kidney disease.
If you or someone you love has been diagnosed with CKD or are experiencing new or worsening symptoms that align with the condition, our experienced and compassionate team is here to help.
We encourage you to schedule an appointment to safeguard your kidney health and get the treatment you need sooner. Prioritize your kidney health and total well-being today.